“Art is not what you see, but what you make others see.” – Edgar Degas
We love this quote because it captures the power of art to reveal that which makes each of us unique. This makes the creation of artwork especially beneficial for individuals living with dementia.
A good example of this can be found in an article published in the National Institutes of Health, which notes several instances where artists developed a depth of emotional expression in their art after being diagnosed with Alzheimer’s disease that was lacking in earlier work. Many well-known artists have continued to produce fine artwork in the years since being diagnosed with dementia. That, by the way, includes many of our Anthem Memory Care community residents who were commercial artists in their earlier years.
And there are many benefits to engaging in art activities for individuals with dementia, including the following:
At our Anthem Memory Care communities, we celebrate the artist in all our residents. We are continually impressed by the patience and care residents take with art projects and by the pride they show in their finished pieces.
Several of our communities participate in a program called Memories in the Making, a unique fine arts program originally created by The Alzheimer’s Association for individuals with dementia. It offers a creative, non-verbal way of communicating and capturing precious moments through art.
Below are just a few beautiful examples of the artwork produced through this program at Highline Place Memory Care in Littleton, Colorado:


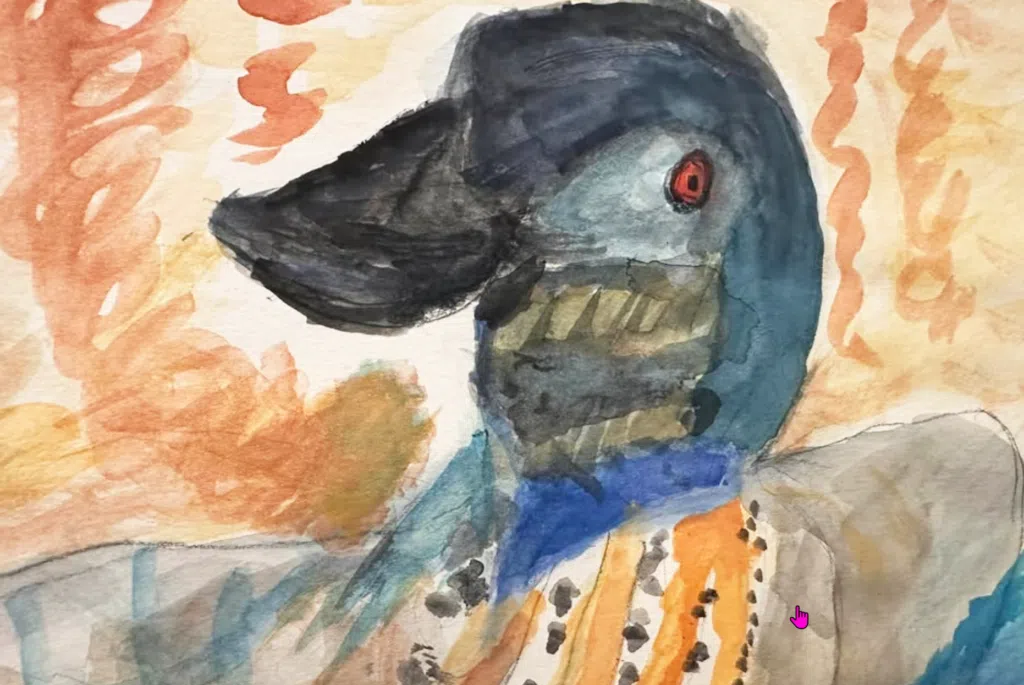
Aren’t these amazing? And this is just a sample!
If you are caring for a loved one with dementia, why not explore some art projects together? The Alzheimer’s Association has some tips to make your artistic endeavors more enjoyable. They include the following:
If you are interested in engaging your loved one in an art project and have some questions, please feel free to reach out to any of our Anthem Memory Care communities. We conduct regular art activities with our residents and would be happy to share our experiences and offer some tips to help you and your loved one experience the joy of creating art together.
(Our header image shows part of the Memories in the Making art display at Highline Place Memory Care. The public was invited in and everyone enjoyed exploring the residents’ artwork.)
Fourth graders from local Cole Elementary in Murrieta, California visited Vineyard Place Memory Care residents armed with their favorite books for a storytime read-along session.
Visits from Cole Canyon students are a regular ocurrence at Vineyard Place that residents and staff always enjoy. Many relationships have grown from these visits which bring positive inter-generational engagement that benefits residents and children alike.
The storytime activity was covered in the local Valley News, which you can read here.
Highline Place Memory Care resident, David Lorenz, worked for 45 years for South Suburban Parks and Recreation in Highlands Ranch, Colorado. And all his years of hard work did not go unnoticed!
Recently, residents and staff of Highline Place hit the road to celebrate David's 82nd birthday. Their destination? David Lorenz Regional Park. You heard that right. The local community named the park in honor of Dave's years serving his communitiy. Some of his co-workers also were on hand for the festivities.
What a great way to celebrate a birthday. Not many can do so with a visit to a park named in their honor!
The event was announced in the local Villager. You can read the details here.
Mary’s day begins with a familiar routine—she wakes up, turns off her alarm and gets out of bed. She takes a shower, washes and dries her hair, applies deodorant, brushes her teeth and gets dressed in a clean blouse and pants. Moving to the kitchen she brews a fresh cup of coffee, pours some juice and enjoys a bowl of cereal. After finishing her meal, she washes the dishes, grabs her keys and heads off to start her day. Later, when she returns home, she’ll change her clothes, prepare dinner, and maybe take a relaxing bath. As the evening winds down, she’ll brush her teeth, wash her face, change into pajamas, set her alarm and get into bed for the night.
Mary is performing her ADLs and IADLs.
Dementia caregivers would refer to Mary’s actions as ADLs (activities of daily living) and IADLs (instrumental activities of daily living). ADLs are the rote tasks most of us perform every day almost without thinking. IADLs involve more complex tasks beyond basic self-care.
For most of us, getting up, using the restroom, calling a friend, buying groceries, cooking meals, and managing our daily lives is something we take for granted. For individuals with dementia, however, IADLS and eventually ADLs will become more and more difficult to manage. At some point, even performing the basic ADLs will become impossible.
Understanding ADLS and IADLs is key to effectively navigating the stages of dementia.
Dr Tamara Cummings is a dementia expert who works with professional caregivers and, among many other aspects of dementia, advises them on best practices used to determine how the stages of dementia impact an individual’s ability to conduct the basic ADLs. Several assessment tools are used in this process, including the Katz Scale, the Lawton-Brody Scale and the Bristol Scale. The Cleveland Clinic has also published a short description of each ADL and IADL.
First, a quick look at the IADLs.
The IADLs will be the first activities that will be impacted by dementia. As mentioned above, IADLs involve more complex cognitive skills. They include the following:
Each of these involves a complex set of skills involving orientation of space and time, verbal abilities, organization, planning, and mobility. At some point you may notice your loved one’s bills piling up unpaid, or they are forgetting to take their medications. These early IADL signs of dementia are important to acknowledge and act upon. Early testing can help optimize your loved one’s access to tools and therapies to keep them healthy as long as possible.
The ADLs are more basic and critical to managing self-care.
At some point, your loved one may begin to find basic rote daily personal care activities more challenging to conduct. For family caregivers, this is a time when more rigorous attention and assistance will be needed.
Here are six basic ADLs to be aware of:
Understanding IADLs and ADLs will help you meet your loved one’s needs more effectively.
Family caregivers of loved ones with dementia will need to understand what ADLs are, how they are impacted by dementia, and how they will need to assist their loved one with their ADLs in the months to come.
We urge you to watch Dr. Tam’s webinar which outlines in detail all the ADLs and the changes associated with the progression of dementia. She has many tips to help caregivers as well.
Feel free to reach out to any of our Anthem Memory Care communities. We will be happy to answer your questions about ADLs and other challenges that you may be experiencing as you strive to help your loved one live their best life going forward. We are always here to help.
Vineyard Place Memory Care in Murrieta, California held a Masquerade Prom --- an evening of dancing, dining, and the selection of Prom King, Skip, and Prom Queen, Sandy. Everyone had a blast, and it brought back memories of high school proms from back in the day!
All this fun was covered in the local Murrieta Patch. You can read the full article here.
Everyone knows that an apple or banana is a healthier snack than a donut or chips. We all understand that there are nutritional benefits from fresh fruits and vegetables that donuts and chips not only lack but can negatively impact health. As a result, we try to make healthy choices with hopes of having healthier bodies that deliver more energy, fewer illnesses, and sharper mental acuity.
Healthy nutrition is even more important for individuals living with dementia. Dementias such as Alzheimer’s disease affect every facet of human health --- cognitive, behavioral and physical. Eating healthy foods is therefore essential to helping them stay as well as possible for as long as possible. Eating unhealthy foods does just the opposite, potentially speeding up the degree of deterioration and negatively impacting their quality of life.
How exactly does healthy nutrition benefit individuals with dementia? Here are five key areas:
The positive impact of good nutrition on the health and wellbeing of individuals with dementia is why it is so important for family caregivers to ensure that their loved ones are adhering to a healthy diet.
The Alzheimer’s Association has some tips to help, which we’ve summarized below:
Above all, never assume that your loved one is eating properly. As the disease progresses their ability to make healthy food choices will become impaired. They may opt for sugary or salty foods. If they are no longer able to cook, they may gravitate towards processed fast foods. At some point, they may even forget to eat altogether. This is why regular supervision of your loved one’s nutrition is essential to keep them healthy and cognitively engaged for as long as possible.
Here are a few additional resources from the Alzheimer’s Association to guide you through the process of providing healthy nutrition for your loved one with dementia:
Feel free to reach out to any of our Anthem Memory Care communities for more tips and resources on healthy nutrition. We’re here to help!
By Lewis McCoy and Isaac Scott
Every memory care community is built on a foundation of compassion, dedication, and love. While beautiful buildings and thoughtful amenities play a role in creating a warm environment, it is those who live and work within it who truly bring a community to life. We want to take a moment to recognize our direct care staff, made up of incredible individuals who devote themselves daily to providing exceptional care for our residents, their families, and each other.

Protecting with Compassion
Our staff are the first line of defense in ensuring the safety and well-being of our residents. They provide more than just assistance with daily tasks; they create a secure environment where residents feel comforted and supported. Whether it's preventing falls, recognizing early signs of medical concerns, or simply offering a reassuring presence, their vigilance and dedication make all the difference.

Engaging with Purpose
Connection is everything, especially in memory care. Our staff understand that meaningful engagement is key to maintaining a high quality of life for residents. From leading music therapy sessions to sharing a quiet moment reminiscing over old photos, they foster joy, dignity, and a sense of belonging. It is their creativity and genuine care that transform everyday moments into cherished experiences.

Loving Unconditionally
True caregivers don’t just perform a job—they form deep, heartfelt bonds with the people they care for. They become trusted companions to residents, sources of comfort for family members, and pillars of support for each other. Their love and kindness create a home-like atmosphere where residents are not just cared for but truly loved.

Hiring for Compassion: The Key to a Thriving Community
The strength of any memory care community lies in its people. Hiring the right individuals—those with a heart for service and a passion for making a difference—can make or break the experience for residents and families. Skills can be taught, but compassion, patience, and kindness come from within. That’s why we focus on hiring those who see caregiving as more than just a job—as a calling.
Here’s to those exceptional human beings who dedicate their talents and compassion to serving memory care residents and who epitomize our Anthem Memory Care mission to “protect, engage, and love”. We honor you.
When a loved one is diagnosed with dementia, it is the beginning of a journey full of changes – physical, cognitive, emotional, and behavioral. Much has been written about these changes and how they relate to the stages of dementia, as well as how to help a loved one adjust and continue to live a purposeful life.
These are all important aspects of navigating dementia that families need to understand to properly care for their loved one. However, not as often addressed are the relationship changes that occur between a loved one with dementia and those they have known and loved all their lives. And, for so many families, those relationship changes can be devastating.
Here are a few of them:
Education is important to fully understand the disease and how it affects everyone.
At our Anthem Memory Care communities, we understand the challenges of this journey. Our communities offer support groups, and we have an abundance of resources to help you and your family navigate these changes together. We encourage you to reach out to us with your questions and concerns. You are not alone—we’re here to help.
February is a month all about hearts. First of all, it’s American Heart Month, which encourages awareness of the importance of heart health. But it’s also the month in which we celebrate the love in our hearts on Valentine’s Day.
Our Anthem Memory Care community residents always look forward to Valentine’s Day because it symbolizes all the years of love they have experienced throughout their lives. And it’s not limited to romantic love. They also enjoy celebrating the loving memories they have of their children, grandchildren and others who have held a special place in their hearts. And Valentine’s Day brings an opportunity for them to reach out to share their love, through acts of kindness with the greater community around them.
Below are some of the special activities our communities have engaged in this Valentine’s season.

At Churchill Place Memory Care in Glen Ellyn, Illinois this lovely couple, along with two others, renewed their wedding vows. Such a touching, heartfelt ceremony!

For residents and families of Willowbrook Place Memory Care in Littleton, Colorado decorated heart shaped frames made perfect Valentine’s Day photo session props!

Big hearted residents of Franklin Place Memory Care in Franklin, Wisconsin used Valentine’s Day as an opportunity to give back by working with Street Angels on Wheels to hold a drive to help the homeless with clothing and hygiene supplies.

A special Valentine’s lunch was held for couples celebrating 40, 50, and 60 years of marriage at Chelsea Place Memory Care in Aurora, Colorado.

At Vineyard Place Memory Care in Murrieta, California it was an opportunity to take a stroll down “Memory Lane” with their favorite local band!
Most of us can remember special Valentine’s Days in our own lives. If you are caring for a loved one with dementia, ask them what Valentine’s Day they remember? Spark their memories by sharing some of your own recollections of handing out valentines in school or getting a surprise bouquet of flowers.
Valentine’s Day may occur one day each year, but with a little encouragement, the spirit of love that it represents can remain with us all year long.
(Don’t you love our header image? This resident of Chisholm Place Memory Care in Wichita, Kansas shares a laugh with the photographer.)
Renewing wedding vows is such a beautiful way to express everlasting love between a couple. At Chuchill Place Memory Care in Glen Ellyn, Illinois three couples renewed their vows in a beautiful Valentine's Day ceremony!
A collection of their wedding photos was on display as the couples walked down the aisle with fellow residents on either side.
The event was covered by the Daily Herald. You can read the full story here:
February is American Heart Month, an opportunity to focus attention on the importance of taking everyday measures to protect and optimize heart health. What you may not know, however, is that there is a clear relationship between a healthy heart and a healthy brain.
That’s why taking some time to understand the role the heart plays in brain health is important. And that includes cognitive health. The National Institutes of Health (NIH) has published studies finding a link between cardiovascular health and cognition. And, yes, the impact of heart disease on the brain can even lead to dementia.
What do we know about the relationship between heart health and brain health?
For the heart to adequately supply blood and nutrients throughout the body, its arteries must be healthy and strong. When they become blocked, every organ of the body quickly becomes impacted. This includes the brain, which requires a steady flow of oxygen-rich blood to function properly. If that blood flow is reduced or temporarily blocked a stroke can occur. When this happens, it can lead to a type of dementia called vascular dementia in which thinking skills are often suddenly impacted after damage to the blood vessels occurs.
The same factors that impact heart health are linked to brain health.
Research cited in a recent Harvard Health article indicates that many of the same risk factors that can lead to heart issues also can lead to dementia. These factors include obesity, high blood pressure, high cholesterol, and diabetes.
And while vascular dementia is most often associated with insufficient oxygen to the brain, newer findings point to heart issues potentially leading to other dementias, including Alzheimer’s.
What can you do to optimize both your heart and brain health?
At our Anthem Memory Care communities, we are big believers in working each day with our residents to keep their hearts and brains as healthy as possible. That means regular exercise, fresh air, brain-healthy foods and an environment that encourages connection with the world around them.
Feel free to reach out to us for answers to your questions and for resources to help your loved one improve their heart health. We welcome you to drop in to visit any of our communities and observe one of our exercise sessions. Our instructors will be happy to give you some tips and additional resources.
Residents and staff of Franklin Place Memory Care in Franklin, Wisconsin are doing their part to provide care and support to the Milwaukee homeless population. They hosted a drive to gather clothing and hygiene essentials for distribution through Street Angels Milwaukee Outreach, a mobile outreach organization that works to bridge the gap between homelessness and housing through advocacy and community collaboration.
Not only are they helping people in need, these charitable acts provide the residents with a renewed sense of purpose and a connection to their greater community.
The clothing drive was covered by the Franklin Patch. You can read the full story here.
Black History Month brings a welcome opportunity for all of us to focus on the achievements and contributions made by Black Americans. And there are many, which cover virtually every area of American life. That includes science and the study of the brain.
Dementia, which we know is a general classification covering several brain diseases that impact memory and physical health and present themselves in different forms. Alzheimer’s disease is the most common form of dementia. It was named after the doctor who discovered the disease, Dr. Alois Alzheimer.
What many people don’t know, however, is that Dr. Alzheimer did not work alone. He assembled a group of the world’s most talented scientists on his journey to discover the cause of this complex, terminal brain disease.
One of the scientists Dr. Alzheimer selected for his team was Dr. Solomon Carter Fuller, a Black African American psychiatrist who had published some of the earliest study findings on dementia.
The Alzheimer’s Association has written in depth about the work of Dr. Fuller. Here are some interesting facts about him:
Dr. Fuller went on to publish what is acknowledged to be the first comprehensive review of Alzheimer’s disease. He has left behind a legacy and a pathway for other Black scientists to follow.
Black History Month helps bring focus on the journeys of Black innovators and visionaries, like Dr. Solomon Carter Fuller. Their talents, perseverance, hard work, and significant achievements continue to serve as a beacon of hope and encouragement for future generations of Black scientists.
(Our header image of Dr. Solomon Carter Fuller was taken from an article on the website of Boston University, which you can access here.)
Residents of Pinnacle Place Memory Care in Little Rock, Arkansas are doing their part to support those impacted by the recent devastating wildfires in Southern California. They are hosting a drive to collect clothing, toiletries and other essentials to help the recovery effort.
Engaging in charitable acts is so important to our Anthem Memory Care residents. It restores a sense of purpose and connection to a worthy cause. We applaud Pinnacle Place and their ongoing efforts!
The drive was covered by the local Little Rock Channel 7 news. You can watch the video here.
Experiencing a sense of meaning and purpose in life is important to all of us. One way to achieve it is by finding ways to give back to those in need. Helping others, as they say, is the best way to help oneself. And nowhere is this truer than for those individuals living with dementia.
The link between experiencing a sense of purpose and improved cognition is supported by several studies. One, cited in the National Institute of Health, found that individuals participating in purposeful acts were able to maintain higher cognitive levels than those who didn’t participate. This included individuals living with dementia.
Anthem Memory Care residents and staff are active within their communities, reaching out to contribute to a variety of worthy causes. Our Pathways of Purpose programs enable Anthem Memory Care residents to engage in activities that connect and engage them in acts that stimulate their awareness of the value of giving back.
That is one of the reasons we encourage families with loved ones with dementia to include them as much as possible in their own participation in fundraisers and other charitable acts.
Below are just a few of our community activities that our residents and staff have enjoyed over this last year.

Chisholm Place Memory Care residents spontaneously hand out rubber duckies to local Target shoppers in Wichita, Kansas. Each ducky had a handwritten positive message. Shoppers were delighted.

This Franklin Place Memory Care resident brings essential food items collected during their food drive to the Hunger Task force in Milwaukee for distribution.

This resident of Cascade Creek Memory Care in Rochester, Minnesota proudly displays some of their hand-made bracelets which were put on sale to raise funds to help Florida hurricane victims.

Residents of Pinnacle Place Memory Care in Little Rock, Arkansas made special “blessing boxes” for their local Food Bank to distribute to families for Thanksgiving.

This resident of Highline Place Memory Care in Aurora, Colorado pets a dog at the local Senior Dog Sanctuary. The residents brought blankets and toys to gift their fellow seniors!
Family caregivers of individuals with dementia can bring this sense of purpose and connection for their loved one through many programs designed especially for their participation. If you are a family caregiver, reach out to your community and look for opportunities to give back to those in need. Include your loved one with dementia on as many of the activities as possible. It can do wonders for their sense of self-worth and yours as well.
Feel free to contact any of our Anthem Memory Care communities for advice and resources. Since we are regularly engaged in community activities we would be happy to connect you to local organizations that are ready and eager to include you in their work.
(Our top image shows a resident of Chisholm Place Memory Care in Wichita, Kansas displaying one of their hand-crafted coasters, sold along with keychains and bracelets as part of a special fundraiser in honor of a local Wichita firefighter, Ty Voth, who was killed in the line of duty.).